When It's Not an Overdose: The Danger of Severe Hypoglycemia in Type 2 Diabetes
- t2diabetesnetwork

- Jul 21, 2025
- 4 min read
Key Highlights
✅ Severe hypoglycemia can appear identical to a drug overdose
✅ Symptoms like seizures, confusion, or unresponsiveness require fast and accurate response
✅ Misdiagnosis can delay care, naloxone won’t help, but glucose or glucagon will
✅ Public awareness is essential, know the signs, act quickly, and reduce stigma
✅ International Overdose Awareness Day (Aug 31) is a chance to broaden understanding

When first responders are called to someone who is unresponsive, seizing, or showing signs of altered consciousness, the immediate assumption is often drug overdose, especially in communities already navigating the opioid crisis. But there's another critical, and often overlooked, medical emergency that can present almost identically: severe hypoglycemia.
This overlap in symptoms is especially relevant in the lead-up to International Overdose Awareness Day (August 31), a global campaign led by the Penington Institute to raise awareness of overdose, reduce stigma, and acknowledge the grief of those left behind. While the day focuses primarily on drug-related overdose, it’s also an opportunity to highlight other critical emergencies that can be mistaken for overdose, like hypoglycemia.
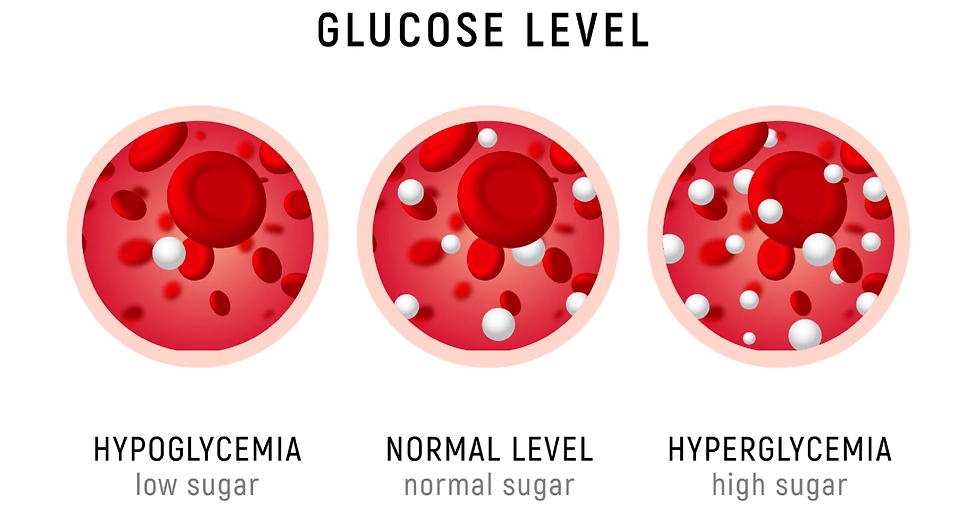
But what exactly is hypoglycemia?
For people living with Type 2 diabetes (T2D), especially those on insulin or certain oral medications, dangerously low blood sugar is a real and persistent threat. According to Diabetes Canada, diabetes-related hypoglycemia results in high cost to the person and the health system in Canada. And yet, this condition often flies under the radar, even among healthcare providers and emergency personnel.
Hypoglycemia/Drug Overdose: Similar Symptoms, Different Causes
Severe hypoglycemia can cause confusion, slurred speech, seizures, loss of consciousness, and in some cases, death, symptoms that closely mimic those of opioid or other drug overdoses. In fast-moving emergency situations, this similarity can lead to misdiagnosis or delayed treatment.
Symptom | Overdose | Hypoglycemia |
Mental Status | Confusion, disorientation, altered consciousness, unresponsiveness, stupor, coma | Confusion, disorientation, difficulty concentrating, irritability, anxiety, unresponsiveness, coma |
Speech | Slurred, incoherent, mumbled | Slurred, incoherent, difficulty speaking |
Coordination/Movement | Dizziness, unsteadiness, poor coordination, staggering gait | Dizziness, unsteadiness, tremors, weakness, poor coordination |
Skin Appearance | Pale, clammy, cool (opioids), flushed (stimulants), sweating | Pale, clammy, sweating |
Heart Rate | Can be slow (opioids) or fast (stimulants), irregular | Rapid or pounding heart rate (palpitations) |
Breathing | Slow, shallow, irregular, labored, depressed (especially opioids) | Rapid, shallow (less common than mental changes) |
Other Notable Signs | Pinpoint pupils (opioids), dilated pupils (stimulants), nausea, vomiting, seizures | Intense hunger, headache, blurred or double vision, tingling around the mouth, seizures |
When blood glucose levels drop too low, the brain becomes starved of energy. This can result in acute neurological symptoms that look indistinguishable from overdose, someone may appear unconscious, unresponsive, or combative.
Why It Matters for People with Type 2 Diabetes
While hypoglycemia is often associated with Type 1 diabetes; but people with Type 2 diabetes who use insulin or sulfonylureas are also at significant risk, especially:
Older adults managing multiple medications
Those with irregular meals or alcohol use
People living alone or with cognitive impairment
Individuals with reduced kidney function
Not everyone experiences hypoglycemia differently. Hear how people with diabetes experience low blood sugar, what triggers their episodes, and how they manage it effectively.
For these individuals, recognizing the early signs of hypoglycemia, shakiness, dizziness, sweating, or confusion, can be lifesaving. But once it progresses to seizures or unconsciousness, quick and correct identification is critical. Delays in treatment can be fatal.
Misdiagnosis Can Have Serious Consequences
Mistaking severe hypoglycemia for a drug overdose can have harmful consequences. People with diabetes may face stigma, judgment, or inappropriate treatment because their symptoms appear drug-related. For example, giving naloxone, a lifesaving antidote for opioid overdose, will do nothing in the case of hypoglycemia. What’s needed instead is immediate glucose administration or glucagon to restore blood sugar levels.
This highlights the need for more informed and nuanced emergency responses that consider diabetes alongside substance use emergencies.

What Needs to Change?
As International Overdose Awareness Day approaches, it’s time to broaden our understanding of what “overdose” can look like, and who it affects. This includes expanding awareness to include conditions like diabetes-related hypoglycemia, which share similar clinical presentations but require entirely different interventions.
Some key opportunities for action include:
Training first responders and healthcare teams to recognize hypoglycemia in addition to overdose
Raising public awareness about the symptoms of severe low blood sugar, especially for caregivers, teachers, and support workers
Encouraging people with diabetes to carry medical ID and have access to emergency glucose or glucagon
Fostering collaboration between harm reduction organizations and diabetes groups to share tools, training, and messaging
Final Thoughts
Severe hypoglycemia is a life-threatening complication of diabetes, and its resemblance to drug overdose symptoms can lead to dangerous delays in care. As we mark International Overdose Awareness Day on August 31, let’s also shine a light on the invisible emergencies faced by people living with Type 2 diabetes, and work together to ensure that all health crises are recognized and responded to with urgency, empathy, and accuracy.
Learn more: International Overdose Awareness Day – August 31
Join us for more interesting insights
Listen to the podcast version of this blog on your phone




